About the PELP Framework
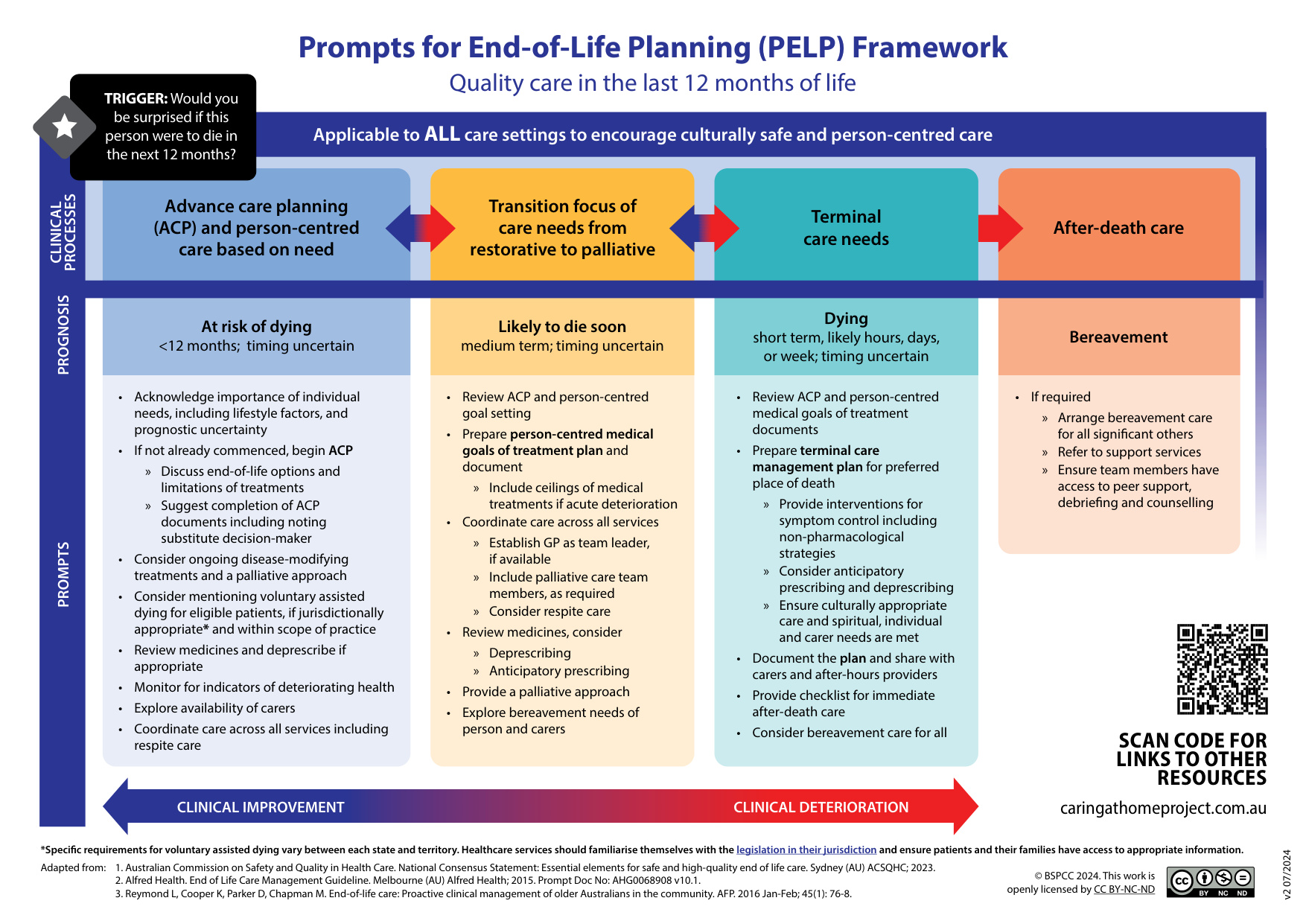
The Palliative and End-Of-Life Care Framework – Last 12 Months Of Life has been updated, including a name change to Prompts for End-of-Life Planning (PELP) Framework.
The Framework guides proactive, quality end-of-life care across all care settings.
The PELP Framework contains prompts that support:
- Identification of patients suitable for a palliative approach to care:
- Ask the surprise question: ‘Would you be surprised if the person died in the next twelve months? This can be answered by intuition , using clinical and personal knowledge of the patient, and/or clinical tools (e.g. SPICT).
- Identification of four clinical end-of-life processes:
- Advance care planning and person-centred care based on need (at risk of dying)
- Transition focus of care needs from restorative to palliative (likely to die soon)
- Terminal care needs (dying)
- After-death care (bereavement).
The PELP Framework
When to use it
Implementation of the PELP Framework helps health professionals deliver quality person-centred care in the last 12 months of life.
It encourages identifying patients at risk of deteriorating and dying, prompting meaningful conversations about their care goals and preferences. These ongoing discussions help create person centred management plans that reflect the person's wishes and reduce making difficult decisions during emotional times.
How the PELP Framework was developed
The framework was recently reviewed by a national advisory committee of GPs, palliative medicine specialists, nurse practitioners and nurses from the following organisations:
- Australian College of Nurse Practitioners (ACNP)
- Australia New Zealand Society of Palliative Medicine (ANZSPM)
- Blue Care - Queensland
- Brisbane South Primary Health Network (BSPHN)
- Consumer representative
- Northern Territory Primary Health Network (NTPHN)
- Rural Doctors Association South Australia (RDASA)
- The Royal Australian College of General Practitioners (RACGP)
Supporting resources
| PELP Section | Title | Description |
|---|---|---|
SPICTTM | Supportive & Palliative Care Indicators Tool (SPICTTM) [PDF 697.22 KB] helps identify people with deteriorating health due to advanced conditions or serious illness. | |
| CareSearchgp App |
The CareSearchgp App offers palliative care information and prescribing guidance to support quality care at end of life and recognising end of life. | |
ACPATM | Advance Care Planning AustraliaTM is a national project enabling Australians to make the best choices for their future health and care. Learn about the process for creating an advance care plan in your state. | |
| QUT End of Life Law in Australia | This webpage discusses the laws on Voluntary Assisted Dying (VAD) both in Australia and internationally, and their intersection with palliative care and medical treatment decision-making. | |
| palliMEDS app | The palliMEDS app familiarises primary care prescribers with eight palliative care medicines that have been endorsed by the Australian & New Zealand Society of Palliative Medicine (ANZSPM) for management of terminal symptoms. The ANZSPM-endorsed medicines can be used to manage common emergent symptoms in home-based palliative care patients in the last few weeks of life when people often have problems swallowing. | |
| Core Medicines | The National Core Community Palliative Care Medicines List (the List) identifies four medicines for use by home-based palliative patients in the terminal phase who require urgent symptom relief. | |
| Gather My Crew app | Set up a 'support crew' with the free Gather My Crew app to coordinate family and friends to help with meals, laundry, grocery pickup or social visits. | |
| HELP App | The HELP App can assist to coordinate the social and practical support that people need when receiving palliative or end-of-life care. | |
| PEPA and iPEPA | PEPA Education provides free health placements in palliative care services and free palliative approach workshops. | |
| Australian Commission on Safety and Quality in Health Care | Identifying goals of care: Tips for clinicians - a Comprehensive Care Standard | |
| Services Australia |
A Advance Care Planning (ACP) and person-centred care based on need
B Transition focus of care needs from restorative to palliative
C Terminal care needs
D After death care
