Most common terminal phase symptoms in uncomplicated palliative care patients can be optimally managed using medicines from the List. | 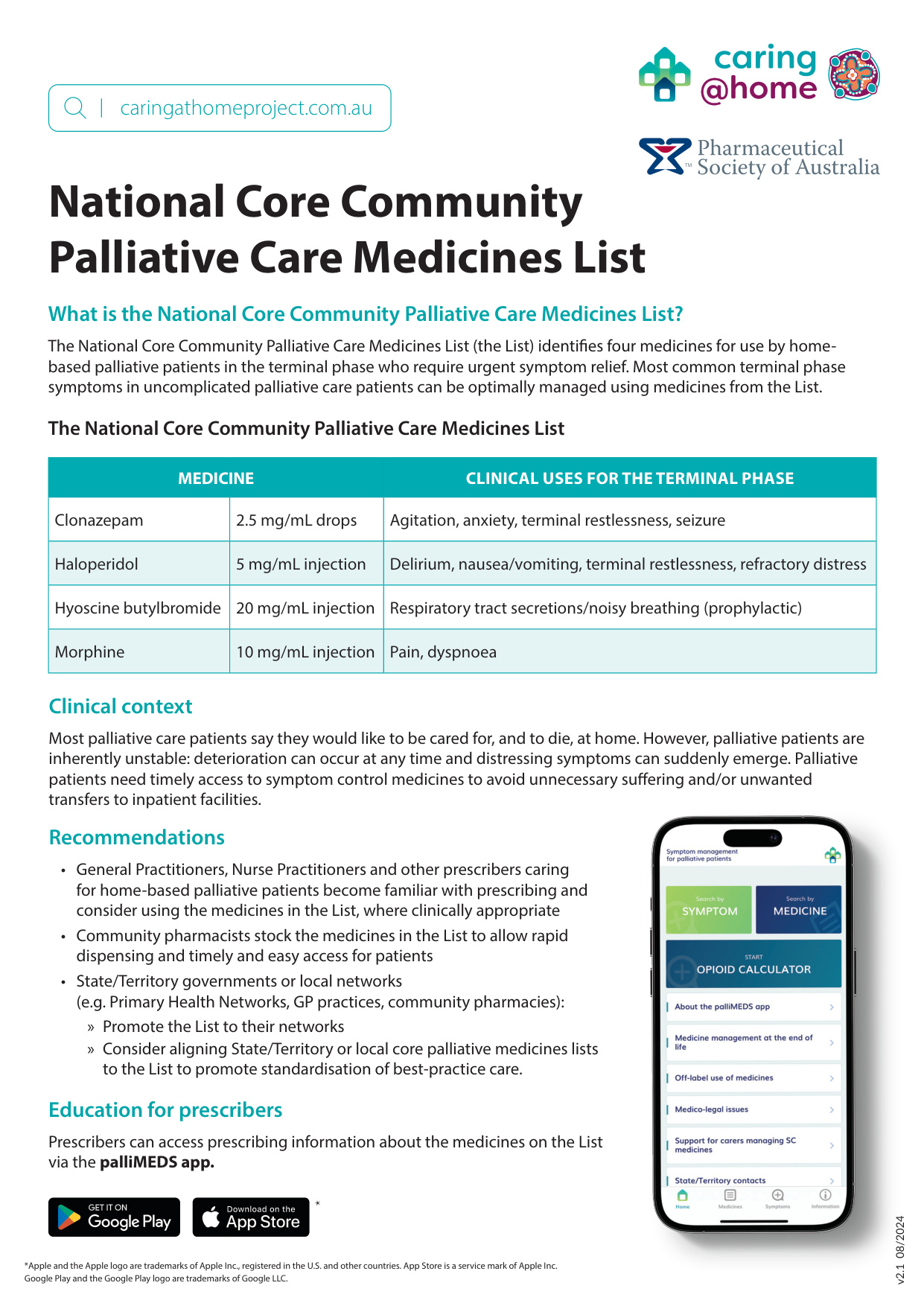 |
| Medicine | Clinical uses for the terminal phase | |
|---|---|---|
| Clonazepam | 2.5mg/mL drops | Agitation, anxiety, terminal restlessness, seizure |
| Haloperidol | 5 mg/mL injection | Delirium, nausea/vomiting, terminal restlessness, refractory distress |
| Hyoscine butylbromide | 20 mg/mL injection | Respiratory tract secretions/noisy breathing (prophylactic) |
| Morphine | 10 mg/mL injection | Pain, dyspnoea |
Clinical context
Most palliative care patients say they would like to be cared for, and to die, at home. However, palliative patients are inherently unstable: deterioration can occur at any time and distressing symptoms can suddenly emerge. Palliative patients need timely access to symptom control medicines to avoid unnecessary suffering and/or unwanted transfers to inpatient facilities.
Recommendations
- General Practitioners, Nurse Practitioners and other prescribers caring for home-based palliative patients become familiar with prescribing and consider using the medicines in the List, where clinically appropriate
- Community pharmacists stock the medicines in the List to allow rapid dispensing and timely and easy access for patients
- State/Territory governments or local networks (e.g. Primary Health Networks, GP practices, community pharmacies):
- Promote the List to their networks
- Consider aligning State/Territory or local core palliative medicines lists to the List to promote standardisation of best-practice care.
Why was the List developed?
In response to requests from key national stakeholders, the Australian Government Department of Health and Aged Care supported caring@home to develop a core medicines list applicable across all Australian States and Territories. The List is a vital tool that will support standardised, quality palliative care by improving access to medicines in the community.
How was the List developed?
Working Party
caring@home convened a national Working Party of clinicians (palliative medicine specialists, rural generalists, general practitioners, nurse practitioners, pharmacists, nurses) with representation from:
- ACT Health
- Agency for Clinical Innovation - End of Life and Palliative Care Network, New South Wales
- Australia New Zealand Society of Palliative Medicine (ANZSPM)
- Australian College of Nurse Practitioners (ACNP)
- Australian College of Rural and Remote Medicine (ACRRM)
- Australian Commission on Safety and Quality in Health Care (ACSQHC)
- Department of Health, Tasmania
- Metro South Palliative Care Service, Metro South Health Queensland
- Northern Territory PHN (NTPHN)
- Palliative Care Australia (PCA)
- Pharmaceutical Society of Australia (PSA)
- South Australia Health
- Safer Care Victoria
- The Royal Australian College of General Practitioners Ltd (RACGP)
- Western Australia Country Health Service (WACHS)
- Western New South Wales Local Health District (LHD).
Working Party guiding principles
The Working Party followed two Guiding Principles to determine medicines to include in the List.
- The List should be informed by the Palliative Care Therapeutic Guidelines, Therapeutic Goods Administration, and existing State/Territory lists of core palliative care medicines.
- Criteria when considering medicines to be included were:
- Evaluation of evidence for management of five symptoms common at end of life
- Consideration of the cost of medicines, including the availability of PBS subsidies
- If there is equivalent efficacy between two medicines consideration of both:
» medicines that can address more than one frequently encountered symptom
» most community friendly form of administration/transport/storage of medicine available.
